With the beginning of a new year, organizations have the opportunity to turn over a new leaf and get their policies and procedures in order. Your physician contracting program may be a prime candidate for review.
An internal audit can provide valuable information on contracting practices and identify opportunities to implement change. Internal audits are periodic, methodical examinations of all contracts and the approval process. They provide an excellent way to document your organization's commitment to compliance. Even if a contract was approved when it went into effect, vague language, complex formulae, lax recordkeeping, and physician relationships can make adherence to your compliance protocols and standards challenging. A periodic, objective and disciplined review of contracts is always a good idea. MD Ranger provides subscribers with web-based tools and reports to make internal audits more efficient and effective.
Goals of an Internal Audit
An internal audit of physician contract payment rates will:
Provide oversight of organization-wide contracting practices. Conducting an internal audit can identify differences in contracting practices and rates across specialties or facilities. It is sometimes difficult to monitor the significance of differences with a large number of contracts that are negotiated by multiple parties; auditing may identify some non-compliant practices within an organization. The typical MD Ranger subscriber has 33 contracts that cost $4.4 million annually for non-employed physician services. MD Ranger provides online reports and tools that make a comprehensive review of key payment rates and hours of service easy to benchmark.Uncover potentially non-compliant agreements. An internal audit can help identify contracts which have payment rates above typical market benchmarks or reveal contracts that need better supporting documentation. An audit can bring these contracts or practices to the attention of your legal or compliance team for further review or documentation at renewal. MD Ranger's tools allow sorting of contracts by where they fall on the market benchmarks, making identification of problematic contracts simple and fast.
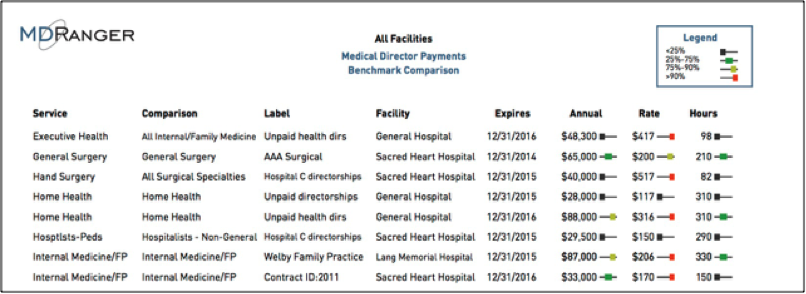
These numbers do not reflect real data from the MD Ranger database.
- Ensure all agreements have appropriate documentation. Most organizations have at least a few unusual contracts that need additional documentation of FMV or a few that didn't go through the proscribed approval or documentation process. The audit will identify the need to improve documentation to show the source of FMV determination when the contract was negotiated and the timing of extensions and amendments. An audit should include a review of time records from physicians that document actual time spent.
- Prevent duplicative services. An audit may reveal medical directorship positions than can be justified, either because multiple people provide substantially similar services or a contract calls for more hours than meets the FMV. Investigate how many directors are commercially reasonable for a service, or if some directors may have a more specific title that is not being adequately described. Unsure how many medical directors make sense per specialty? Use MD Ranger's Number of Administrative Positions per Service table for a gut check.
- Check that approval process is working. Review the records for contract approvals to ensure that all contracts are processed appropriately.
- Verify all contracts are current. Stark requires payment rates to be set in advance; hence it is important that contract renewals are processed prior to expiration. Be sure extensions are in place if contract negotiations are going to extend beyond the expiration date.
Check back next week for approaches to auditing.


.svg)
.svg)
.svg)
.svg)