With the beginning of a new year, organizations have the opportunity to turn over a new leaf and get their policies and procedures in order. Your physician contracting program may be a prime candidate for review.
An internal audit can provide valuable information on contracting practices and identify opportunities to implement change. Internal audits are periodic, methodical examinations of all contracts and the approval process. They provide an excellent way to document your organization's commitment to compliance. Even if a contract was approved when it went into effect, vague language, complex formulae, lax recordkeeping, and physician relationships can make adherence to your compliance protocols and standards challenging. A periodic, objective and disciplined review of contracts is always a good idea. MD Ranger provides subscribers with web-based tools and reports to make internal audits more efficient and effective.
Approaches to Auditing
The Bottom-up Audit
The bottom-up approach is the most traditional an audit method, entailing a review of each contract for adequacy of FMV documentation, time records, and renewal/approval process.
The MD Ranger contract summary report provides subscribers with a line-by-line report of where each of their contracts fall compared to MD Ranger benchmarks. This provides a quick way to identify higher risk contracts. Several MD Ranger subscribers use this report annually to document their internal compliance review of physician contracts.
The Top-down Audit
The top-down auditing approach looks at an organization's contracts and physician contracting compliance process as a whole to assess whether there may be underlying issues with the process, such as duplicate or excessive payments to individual physicians or groups. The process can be an effective tool for financial management and budgeting, as well as providing support for negotiations through comparisons in rates across specialties, consistencies, etc.
A few suggestions if you audit in aggregate:
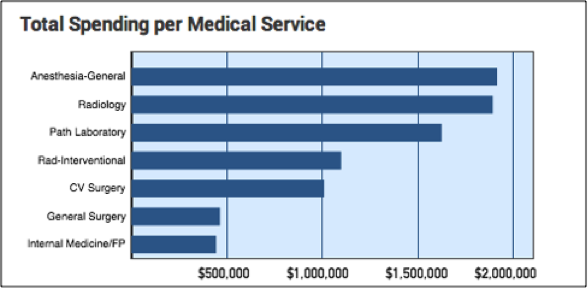
- Review how much is being spent per service (Neurology, Cardiology, etc.) across all types of agreements (administrative, call coverage, leadership, etc.).
- Determine if the number of medical directors for each specialty/service is appropriate and within market ranges.
- Examine the combined revenues from net professional collections plus stipends for hospital-based services.
- Review specialties where all administrative or coverage contracts are staffed by a single physician or one practice to be sure payments do not exceed market rates for actual time committed, or if the physician cannot be reasonably expected to dedicate the minimum number of hours while maintaining their clinical practice load.
- Multi-campus deals need particular documentation for time required.Documentation of competitive bidding and a Request For Proposal process in contentious/excessive situations.
How Often Should Audits Occur?
Your organization may already have a policy for conducting periodic internal audits, thus the initial step is to document that the process is being followed. If there is no policy, investigate how other departments and business functions are audited at your organization. Depending on your facility and how your physician agreement terms are organized, audits can be annual or biennial. Whether routine or ad hoc, an internal audit is a valuable process for documenting a strong compliance process and identifying potential risks to your organization.


.svg)
.svg)
.svg)
.svg)